Personalized medicine by optimal prescription of treatment
Ex of projects:
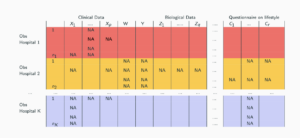
- Optimal individualized treatment regime of plasma transfusion for severe trauma (superlearner with missing values)
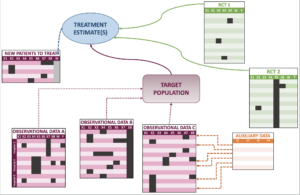
- Survival causal inference when combining RCT and observational data (from estimating the RMST to defining optimal policy)
- Variables selection when transporting the causal effect from an RCT to a target population
- Sensitivity analysis when identifiability assumptions are violated
- Dynamic treatment regimes with missing values
Personalized medicine by integration of different data sources
Ex of projects:
- Measures of dependencies between random vectors
- Handling (Informative) missing values in time series structured by blocks
- Predictive intervals for machine learning algorithms (with missing values)
- Federated learning: collaboration between hospitals
Application context
Beyond methodological developments, innovative responses to the public health challenge first posed by respiratory allergies are targeted. For more than 30 years, there has been an increase in a number of chronic non-communicable diseases (NCD), such as asthma and allergies, respiratory diseases. Allergies are the fourth most common chronic disease in the world. The World Health Organization (WHO) predicts that by 2050, one in two people in the world will suffer from allergies (Bousquet, 2009; inserm press). In France, the number of people suffering from allergies has doubled in 20 years, particularly among children and young people. Although the expression of these diseases results from the interaction between the genetic background and the environment, especially through epigenetic mechanisms, their sudden increase is solely due to the environmental changes that occurred in the last decades because of the Western lifestyle, the genetic heritage requiring centuries to change. Reaching a better understanding of the complexity of chronic NCD, requires analysing large heterogeneous data.
There is a gap between the numerous ML methods developed and what is currently used in practice. In a review paper on ML in the field of allergy based on a bibliometric analysis over the past 50 years, Fontanella et al. (2021) have noted that only 15% of the 3000 articles which use data analysis, resort to ML tools, that are quite simple (1.7\% use random forest and 0.9\% use deep learning tools). They also highlighted that “very few research findings have been translated into clinically actionable solutions”. The lack of confidence in these new tools may be due to a lack of interpretability (black box effect), of uncertainty quantification, of reproducibility and of practitioner’s training. The sequential work between clinicians and methodologists rather than involvement of both parties at each stage of development, is another limitation. Nevertheless, a major lock is the lack of consultation, discussion, involvement of all stakeholders and regulators.
Fontanella et al. (2021) have also called for collaborative science and great care when analysis results to avoid blindly trusting the results of the algorithms; all these components are at the core of PreMeDICaL.
Ex. of projects:
- Benralitrap project. CT air-trapping characterization for the early identification of Benralisumab responders among eosinophilic asthma patients
- CRO-AIT project: Combining Allergen ImmunoTherapy Randomized controlled trials and Observational studies (project with ALK)
Projects
You can apply for research positions as part of these projects: contact Julie Josse and Aurélien Bellet.
PEPR (Priority Research Program and Equipment)
SMATCH 2023-2029
Statistical and AI based Methods for Advanced Clinical Trials CHallenges in Digital Health
The project is structured around several work packages on the following topics:
1️⃣ New clinical trial methods and designs based on the transition from animal to human, research-based disease models,
2️⃣ Enriching clinical trials with multi-source and multi-dimensional ancillary data,
3️⃣ Next-generation designs for the clinical evaluation of digital medical devices based on AI algorithms,
4️⃣ Regulation, feasibility and dissemination of clinical trials
With Inria project-teams: HEKA, SISTM, SODA.
DIGPHAT 2023-2027
Digital Pharmacological Twins
Keywords: Pharmacology, multi-scale, digital pharmacological twins, therapeutic drug monitoring, pharmacogenomics, molecular modelling, dose individualization, transplantation, anti-infectious, oncology
With Inria project-teams: HEKA and COMPO.
SSF-ML-DH 2023-2027
With Inria project-teams: EPIONE and PRIVATICS.
Inria challenge
FedMalin 2022 – 2026
FEDerated MAchine Learning over the INternet
Aurélien Bellet & Giovanni Neglia
In many use-cases of Machine Learning (ML), data is naturally decentralized: medical data is collected and stored by different hospitals, crowdsensed data is generated by personal devices, etc. Federated Learning (FL) has recently emerged as a novel paradigm where a set of entities with local datasets collaboratively train ML models while keeping their data decentralized.
FedMalin is a research project that spans 11 Inria research teams and aims to push FL research and concrete use-cases through a multidisciplinary consortium involving expertise in ML, distributed systems, privacy and security, networks, and medicine. We propose to address a number of challenges that arise when FL is deployed over the Internet, including privacy & fairness, energy consumption, personalization, and location/time dependencies.
FedMalin will also contribute to the development of open-source tools for FL experimentation and real-world deployments, and use them for concrete applications in medicine and crowdsensing.
The FedMalin Inria Challenge is supported by Groupe La Poste, sponsor of the Inria Foundation.
With Inria project-teams: MAGNET, NEO, COATI, COMETE, DYOGENE, EPIONE, MARACAS, SPIRALS, TRIBE, WIDE