Funding
IDeaS is a project funded by ANR (french research agency) under the grant #JCJC-SIMI-3. It involves researchers from the Shacra Team (LIFL – INRIA LNE) and researchers from the Magrit Team (LORIA – INRIA Lorraine).
Participants
- Defrost Jeremie Dequidt (Coordinator)
- Defrost Christo Gnonnou
- Defrost Mario Lopez
- Defrost Christian Duriez
- Mimesis Stephane Cotin
- Magrit Erwan Kerrien
- Magrit Marie-Odile Berger
- Magrit Ahmed Yureidini
- C.H.U René Anxionnat
Project Rationale
Cerebrovascular diseases are reported to be one of the most common causes of death worldwide with 9.3% of total deaths (source: World Health Organization, October 2008). Interventional radiology is a specialty of radiology that is able to treat such diseases with minimally invasive procedures through image guidance. A thin flexible tube called catheter is inserted into the femoral artery through a small puncture in the groin. The catheter is used as a conduit to guide other therapeutic devices (guide-wires, coils, stents…). These neuro-interventional tools are pushed, pulled, rotated by the surgeon to navigate in the vascular network to reach the damaged area.Guidance is performed using X-ray imaging. Flat panels X-ray detectors allow for X-ray image acquisition framerates up to 30 frames per second, with low radiation dose, that can be displayed in real-time onto a set of in-room monitors. Such image acquisition protocol is called fluoroscopy. An X-ray opaque (iodinated) contrast medium is injected through the catheter to allow for revealing blood vessels.
Benefits of minimally invasive procedures are not questionable: patient safety is increased as morbidity, infection risk, physical trauma are lowered but the economic cost is also reduced when compared to open-surgery. However, major limitations to the technique exist. First, even if performed at low dose rates, the length of interventional radiology procedures may lead to a high absorbed dose for the patient. Furthermore, low-dose Xray cannot but provide a poor visual feedback, with a low signal to noise ratio and low contrast, and where blood vessels cannot be seen but at times at the cost of a contrast medium injection. And finally, the third dimension, the depth, is completely lost within such a 2D, planar, imagery. Biplane systems exist but are still rare, and cannot raise all difficulties to infer the 3D shape of tools or complex vascular structures.
Computer simulation is a common and efficient tool to predict the behavior of a real phenomenon. However the accuracy of a simulation and its predictive capabilities really depend on the modeling of the system. For simple phenomena, models exist that can faithfully describe the underlying system with equations. However for complex phenomena or complex procedures, models tend to diverge from what is observed in reality or even are not robust enough to be useful. Despite their mathematical complexity (non-linearity for instance), models are defined based on the observations within a simple environment and benchmarked or validated with the same simple environment. When associated with complex environment (like a catheter moving in vascular network), those models exhibit their limitations. A strong requirement for this proposal is to have simulation models that are able to produce outputs that can be super-imposed to real data and thus do not diverge from what is expected.
IDeaS is a fundamental research program targeted at per-operative guidance for interventional radiology procedures. Our main goal is to provide effective solutions for the two main drawbacks of interventional radiology procedures, namely: reduce radiation exposure and provide a fully 3D and interactive visual feedback during the procedure. To do so, our project relies on an original combination of computer vision algorithms and interactive physics-based medical simulation. Computer vision algorithms extract relevant information (like the actual projected shape of the guide-wire at any given time) from X-ray images, allowing adjusting the simulation to real data. Conversely, computer-based simulation is used as a sophisticated and trustful predictor for an improved initialization of computer vision tracking algorithms.
Many outcomes may be expected both in scientific and clinical aspects. On the scientific side, we believe a better understanding of how real data and simulation should be merged and confronted must lead, as a natural by-product, to image-based figures of merit to actually validate computer-based simulation outputs against real and dynamic data. A more accurate identification of the factors limiting the realism of simulation should follow with a rebound impact on the quality of the simulation itself. An actual integration of a mechanical model into the loop will improve the tracking. We firmly believe mechanical constraints can supplement the image data such that dynamic single view reconstruction of the interventional devices will be possible. On the clinical side, using the prediction capabilities of the simulation may decrease the need for X-ray images at high rates, thus leading to lower exposure to radiations for the patients and surgical staff. Finally, the output of the simulation is the 3D shape of the tool (e.g. guide-wire or catheter), but not only. Additional information may be visualized, for instance pressure of the catheter on the arterial wall, to prevent vessel wall perforations, or reduce stress on the arterial wall to prevent spasm. More generally, richer information on the live procedure may help surgeons to reduce malpractice or medical errors.
Results

Tracking device for interventional radiology tools.
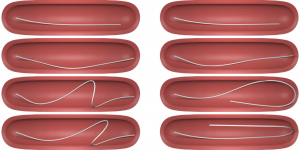
Simulation of catheter and its contact model. These images highlight the role of friction in the catheter deployment.
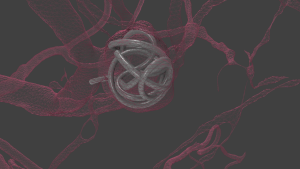
Simulation of a coil in an aneurysm

Simulation of a coil in an aneurysm (Simulated X-ray image)
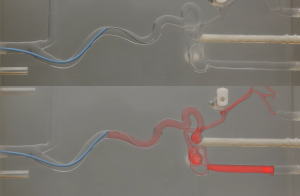
Deployment of a real catheter in a silicone phantom vs deployment of a simulated catheter


